We Deliver Expertise with Heart, Every Day.

We will find you the perfect fit.
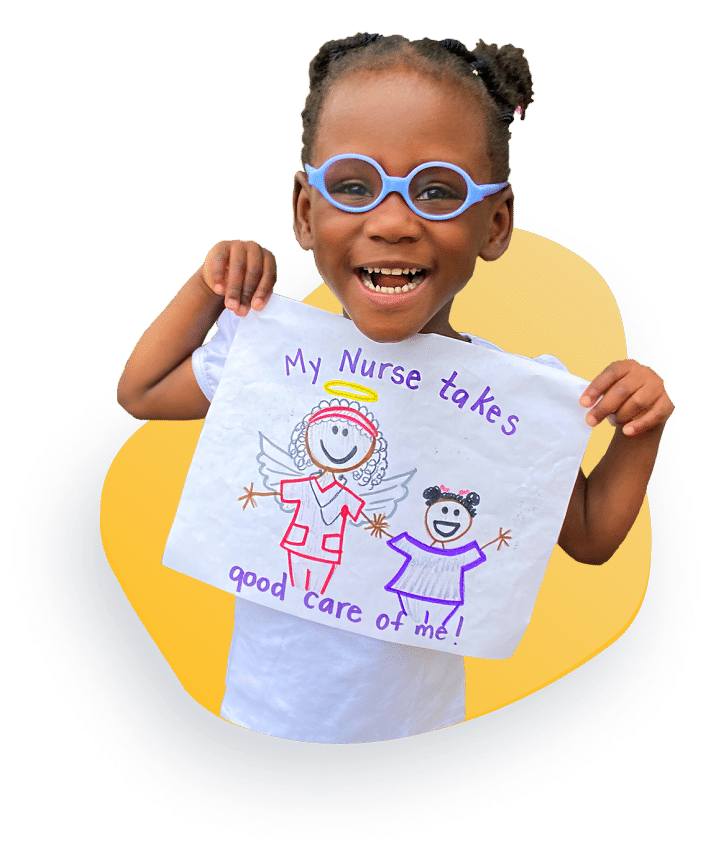
Our goal is to provide the best home health care and to serve you in a loving, caring, and professional manner. We infuse our “HALOS” values (Heart, Advocacy, Love, Outreach, Speed) into everything we do, with our clients at the Heart of every decision. We are a big family here, so we pour into our employees; we feel when we show love to our employees and they love their job, they will pass that love onto our clients.
The Angels of Care family includes thousands of HALOS-minded nurses, therapists, attendants, CNAs, and specialists throughout the states we serve, and we would be honored to match you with the perfect clinician to care for your loved one.
Testimonials
Lives Our Angels Have Changed
Hear from families like yours who’ve trusted the Angels for their care.
Call us Today for More Information!
Angels of Care is The Name You Can Trust for Pediatric and Young Adult Nursing, Home Health, Therapy, and Support Services.




